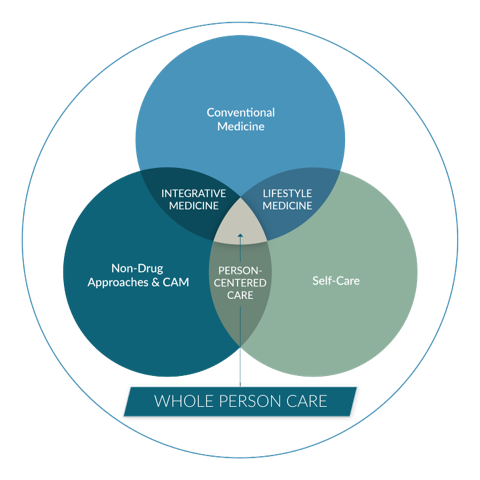
Whole Person Care
Healing Works Foundation’s mission is to make whole person, integrative care regular and routine.
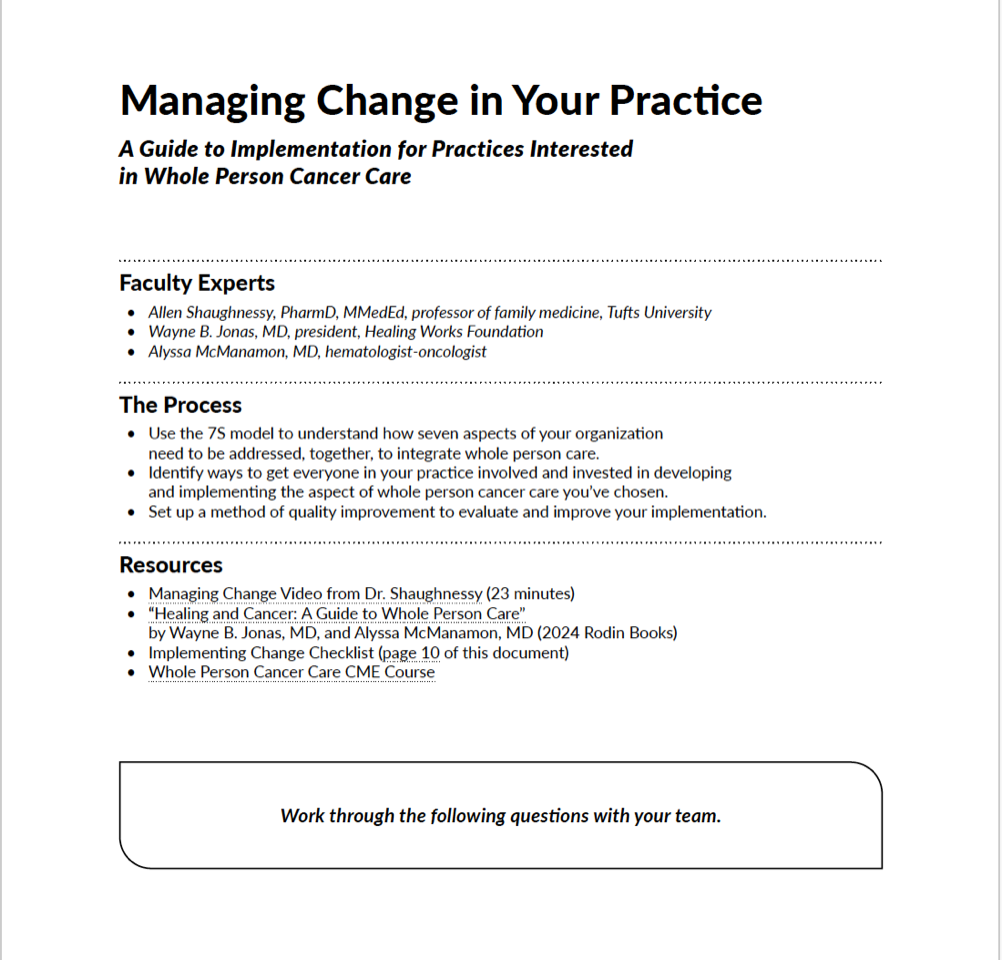
Led by Dr. Wayne Jonas, HWF partners with a diverse group of wellbeing innovators. It creates platforms, processes, programs, tools and services to support and magnify insights and innovations in healing and whole person care principally in primary care and oncology.
Healing Works Foundation Blog
You Already Know How to Do Whole Person Care
An excerpt from Healing and Cancer: A Guide to Whole Person Care If you've never (until reading Healing and Cancer) heard of the Personal Health Inventory (PHI) as a tool or the HOPE visit as…
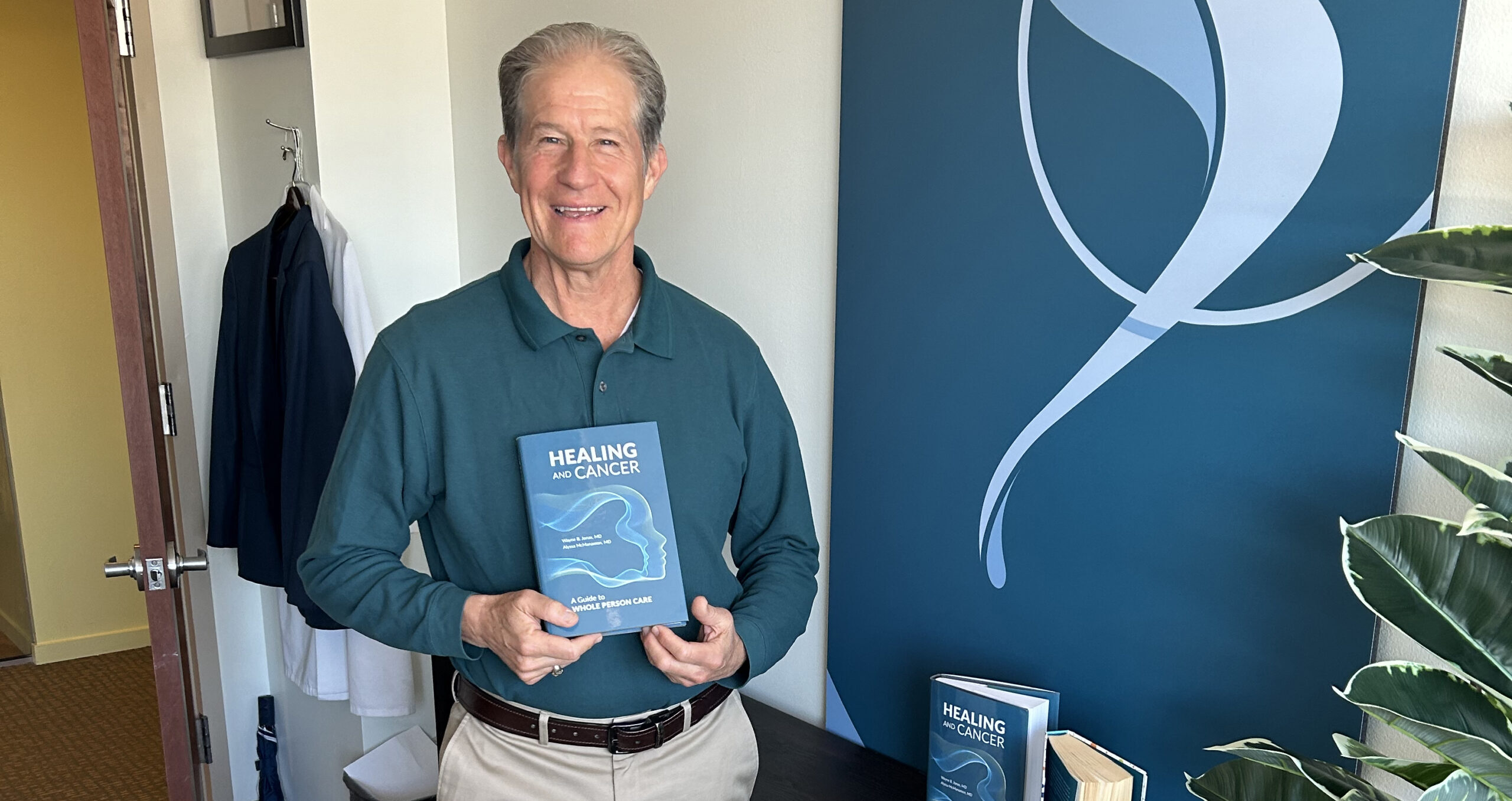
Announcing My New Book: Healing and Cancer
Navigating the complexities of oncology care often means addressing more than just the clinical aspects of cancer. Conventional healthcare models, with their focus on symptom management and disease treatment, sometimes miss the holistic needs of…
How to Measure Nothing
In health care, if you do not name and document a problem or a process, it remains invisible. It might as well be nothing. The biggest problem we have for improving health and lowering the…